CNS Value Story Analytics: An Independent Study
By providing comprehensive, multidisciplinary therapy, Centre for Neuro Skills (CNS) may reduce monthly healthcare cost in the long-term, reduce overall prescription drug expenditure, and improve patient outcomes by reducing hospital re-admissions and emergency room visits. A detailed third-party analysis was provided comparing CNS to similar facilities and other alternative patient care journeys. Data was gathered and analyzed by this third-party consultant and consisted of 15 million healthcare claims [covering more than 1 million individuals] over a 5-year period. The consultant is not affiliated with the Centre for Neuro Skills.
Patient Demographics
UHC and Blue Cross/ Blue Shield claims were reviewed and filtered for relevant brain injury diagnoses. A total of 15 million claims covering over 1 million patients across several patient journeys were included in the sample. The analysis period included 1-year pre-index event, the index year, and 3-years post-index year, for a total of 5-years. Data was focused on monthly cost, prescription drug expenditure, and hospital admissions/ER visits. Injury severity was classified based on review of the diagnosis as identified through corresponding diagnosis codes.
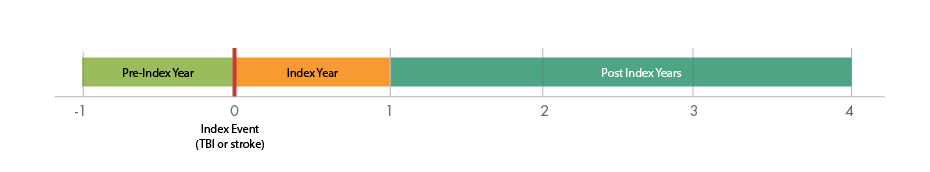
See Fig 1. and Fig 2. for patient profile details.
Fig 1. Patient Profile
How CNS patients compare to patients in other patient journey models
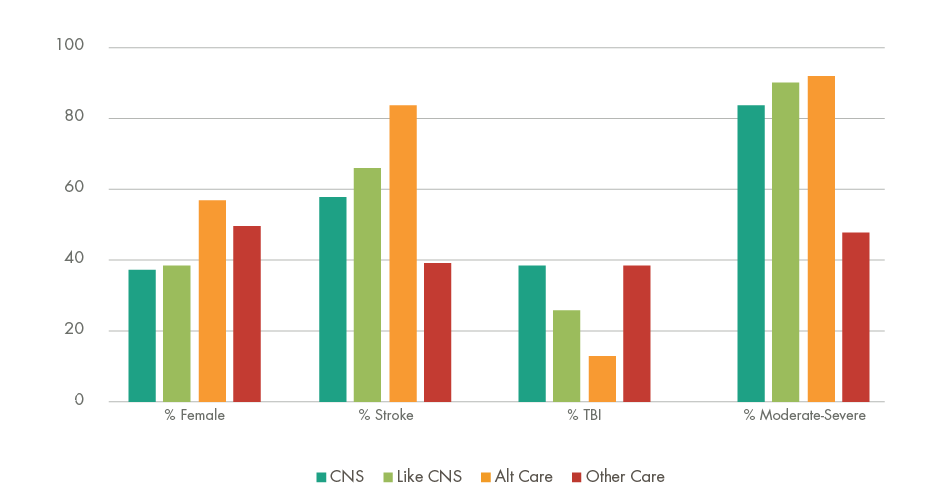
Alternate Care: Skilled Nursing/LTAC/IRF
- More than 85% of CNS, Like-CNS, and Alternate Care patients have moderate-to severe injuries.
Fig 2. Patient Profile
How CNS patients compare to patients in other patient journey models
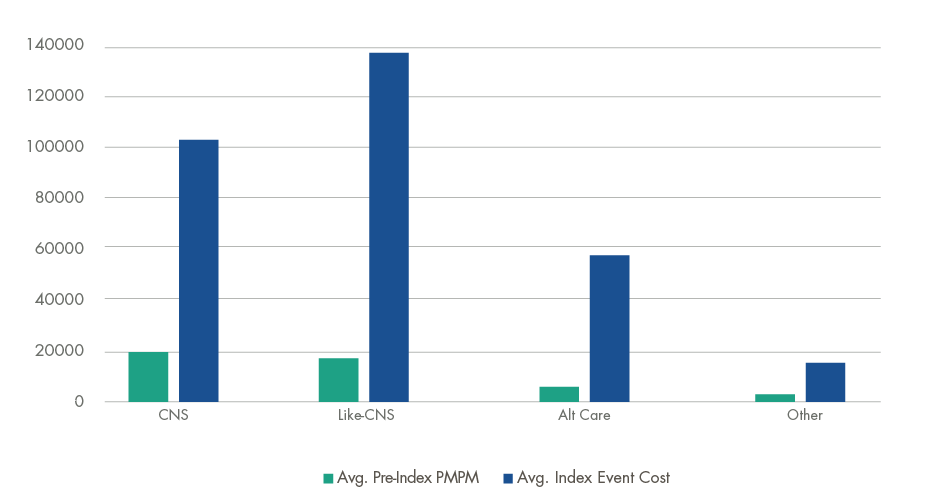
- CNS patients had the highest pre-index monthly cost (14% higher than Like-CNS), indicating more medically complex patients at the time of injury and admission to CNS.
Monthly Cost
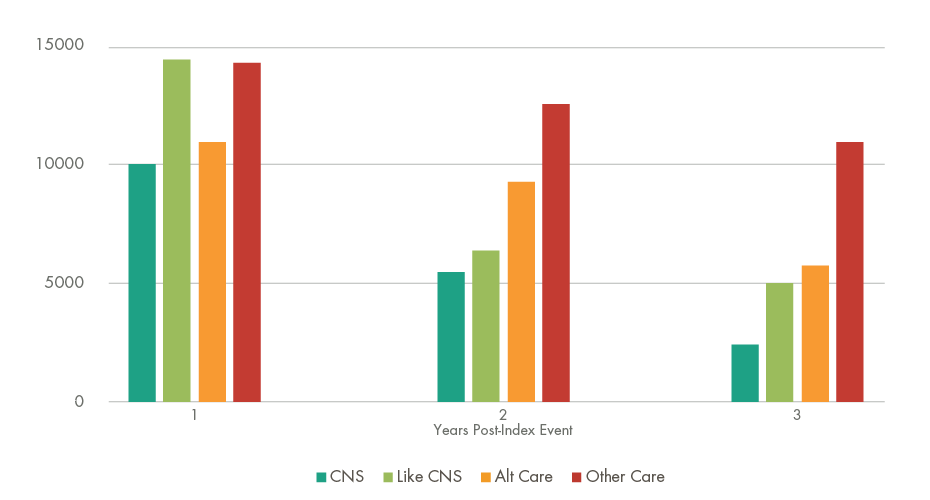
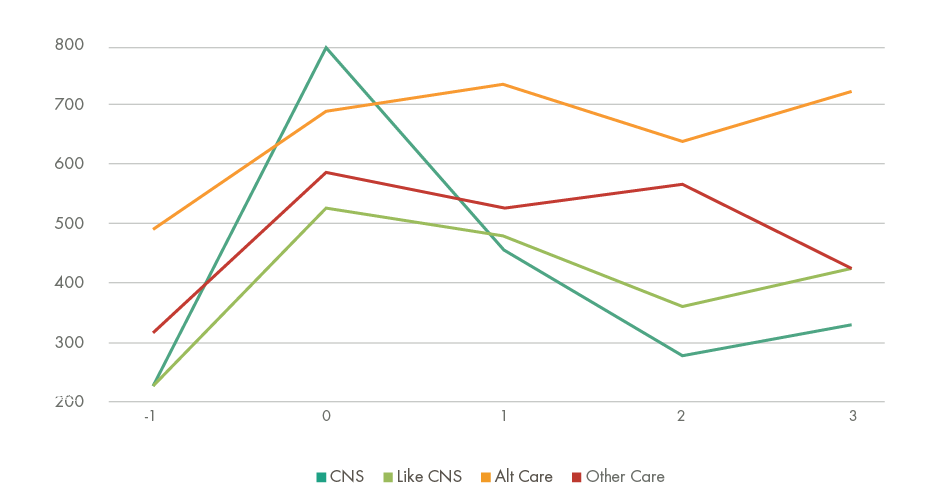
Of all patient journey models, CNS patients had the highest average monthly cost in the index year (i.e. the 12 months following the brain injury event); however, by the 3rd year post-index event, the average monthly cost for CNS patients was the lowest of all patient journeys (30% less than Like-CNS facilities). This represents a 71% decrease in cost in the 3-year follow-up period, which is the most substantial decline in cost of all patient journeys that were analyzed (Fig 3.).
Fig 3. CNS Patients Monthly Cost Decreases 71% Post-Index Event
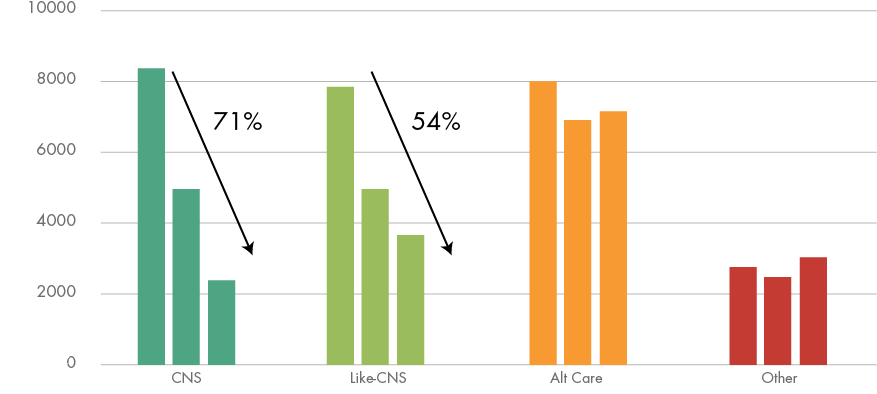
- CNS patients exhibited the most substantial decline in monthly cost of all patient journeys. By year 3, CNS patient monthly cost was 30% lower than Like-CNS.
When segmenting the data by total therapy cost (overall cost of therapy >$100k), CNS patient monthly cost remained the lowest in all 3 years following the index event; translating to immediate cost savings (Fig 4.). By year 3, CNS patient monthly cost was 46% lower than Like-CNS facilities, a savings of over $26k per member in that year alone, and was 77% lower than “Other Care/No Care” options, a savings of over $100k per member that year.
Fig 4. Monthly Cost Savings of Over $90k (Compared to Like CNS) Post-Index Event
- In the 3-years post-index event, CNS patients saved over $90k when compared to Like-CNS and Alt Care patients, and over $230k compared to Other Care options.
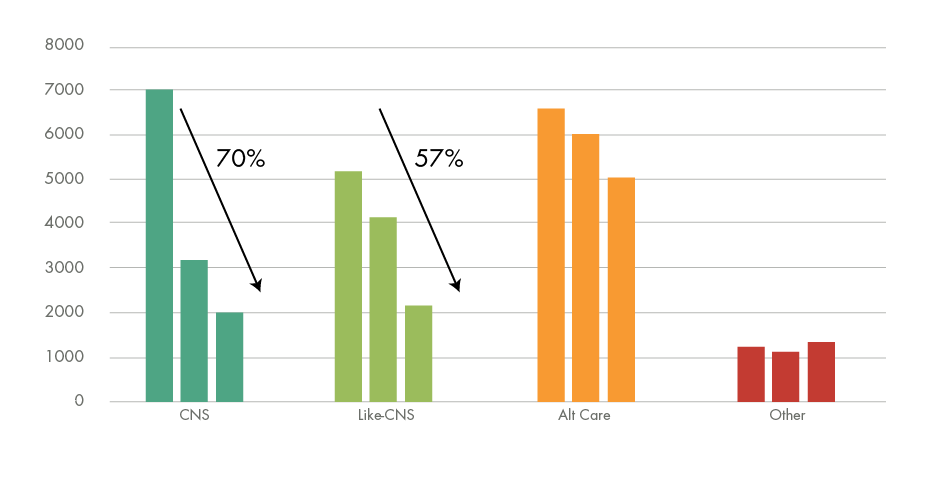
Evidence of monthly cost reduction was also seen within stroke and TBI injury types separately. CNS stroke and TBI patients each exhibited a 70%+ reduction in monthly cost in the 3-year follow-up period, vs. 47% and 57% respectively for Like-CNS facilities (Fig 5A. and Fig 5B.).
Fig 5A. CNS Stroke Patient Monthly Cost Decreases 74% Post-Index Event
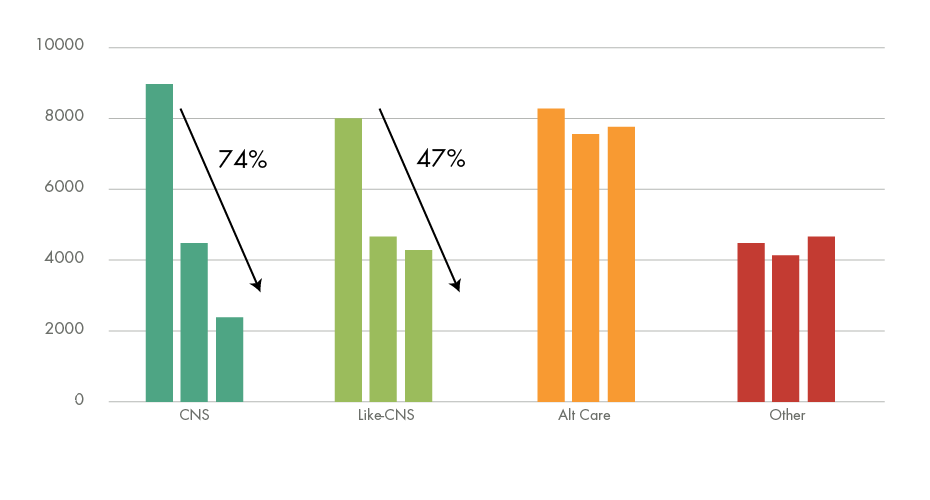
Fig 5B. CNS TBI Patient Monthly Cost Decreases 70% Post-Index Event
Prescription Drug Expenditure
Post-index, CNS patients saved an average of $220 per month compared to Like-CNS patients. CNS patient prescription drug cost dropped 34% ($242/month) in the first year alone [following the index event], vs. a 15% ($73/month) decrease in cost for Like-CNS patients (Fig 6.).
Fig 6. CNS Rx Drug Cost Decreases 34% in the First Year Post-Index Event
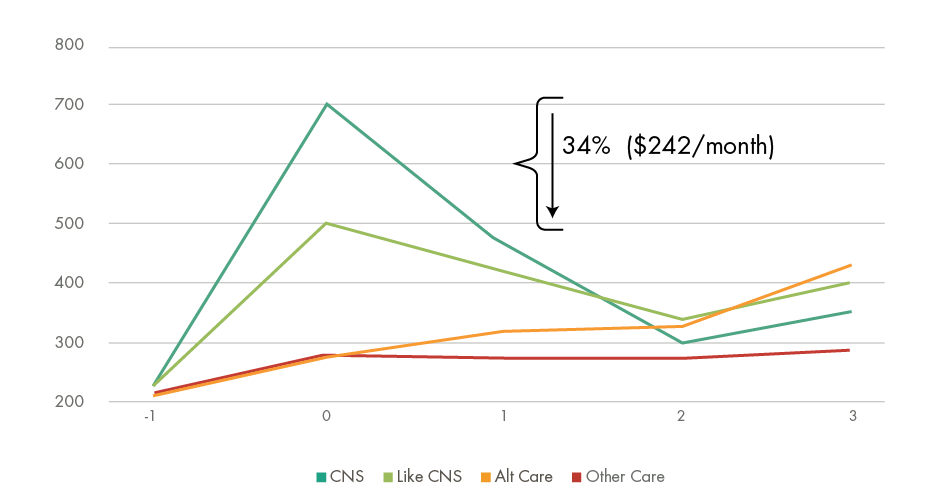
- In the index-year, CNS patients had the highest monthly prescription drug cost; however, average drug cost dropped 34% in the first year alone (49% overall). This was the largest decline in prescription drug cost of all journey models analyzed.
For those patients with >$100k in therapy cost, CNS patients saved an average of $446 per month on prescription drugs in the 3-years post-index event, which is 6x more savings than similar patients at Like-CNS facilities ($73/month) (Fig 7.).
Fig 7. CNS Patients Save 6x More than Like CNS on Prescription Drugs (Post-Index)
- CNS patients’ prescription drug costs were the lowest of all patient journey models beginning the first year after the index-event.
Outcomes
Cumulatively, in years 1-3 post-index event, CNS patients had the second lowest percentage of patients with a hospital admission (20.2%), second only to “Other Care” (20.1%); however, the percentage of CNS patients with hospital admissions declined 85% from the index year.
For patients spending >$100k on therapy, the percentage of CNS patients with a hospital admission was approximately 50% lower than Like-CNS and Alternate Care facilities. Emergency room visits were also the lowest for CNS at 38.5%. CNS was more efficient at reducing hospital admissions/emergency room visits across the continuum, having the lowest number of admits per 1,000 by significant margins. Admits per 1,000 is a common measure of a hospital, healthcare center, or treatment facility’s efficiency. This value represents the number of member claims with inpatient admissions/emergency room visits for every 1,000 claims.
CNS Patients have Reduced Admits per 1,000 and ER Visits per 1,000 by Significant Margins
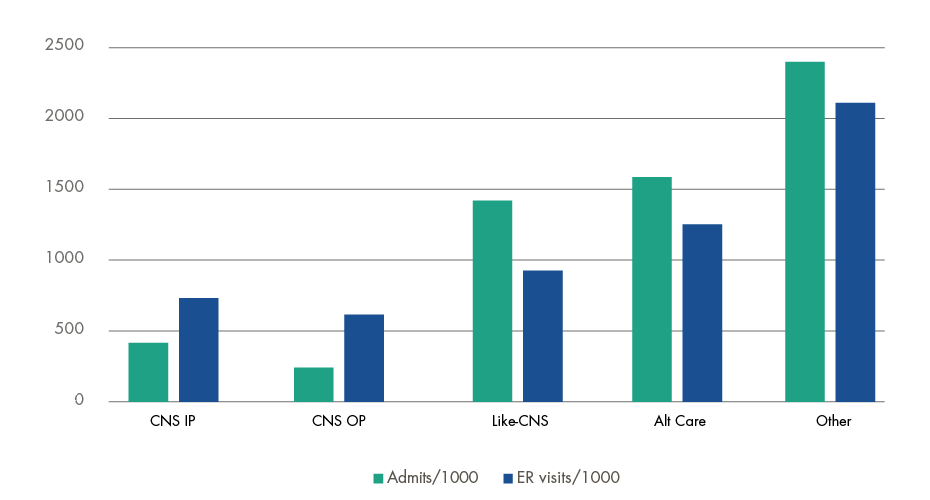
- CNS inpatients had 67% less claims with inpatient admissions and 14% less emergency room visits than Like-CNS facilities.
Investment in Rehabilitation Reduces Overall Cost
In summary, while a higher proportion of CNS patient monthly cost is related to therapy, the long-term result is an overall reduction in cost. Data shows that patients come to CNS with higher pre-index monthly and prescription drug costs; however, data also shows that those costs are drastically reduced in the first year after the index-event. This sharp decline in cost does not occur in the other patient journey models and represents an objective measure of CNS’ commitment to patient care. By investing in world-class, multi-disciplinary therapy with CNS, monthly cost consists primarily of concrete and objective methods of improving outcome rather than on acute needs, which remain high throughout the continuum.

